Table of Contents
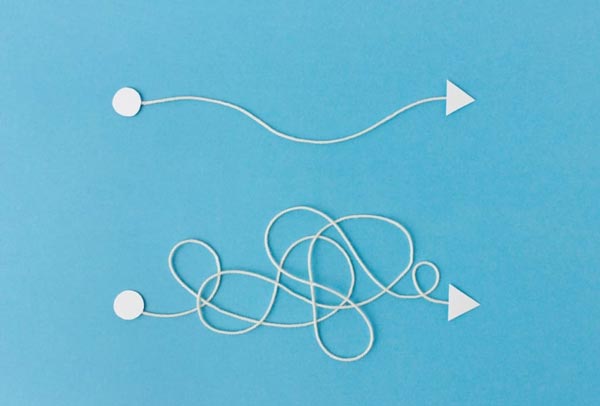
At its core, the conversation around addiction prevention versus addiction intervention reflects a similar dichotomy in medical circles: prevention vs. cure.
Everyone knows the adage: prevention is better than cure. But in the case of addiction, it’s not quite so clear-cut and simple.
The thing about addiction is that you have to approach it as both a societal issue and an individual medical condition. To society, prevention is the absolute priority – effective prevention, that is. To the individual, prevention doesn’t always work – and in some cases, the problem isn’t even identifiable until intervention is the only viable option.
Then there’s the consideration that preventing addiction without impeding on the liberties of an individual presents a challenge, and in some cases, legal or institutionalized measures taken to prevent substance abuse – such as addiction stigma, crackdowns, heavy criminalization, etc. – only seem to cause more harm, and create a different subset of issues around drugs and society as per DrugPolicy.org.
That doesn’t change the fact that prevention is necessary and integral to lessening the detrimental effects of drug addiction in society, but the way we approach preventing addiction has to be changed from the ground up.
To begin with, we must all recognize that prevention and intervention are both important – but under different circumstances, one is more important than the other. But before we look at how that works, it’s important to tackle one critical aspect of addiction: why it starts.
Understanding The Risk Factors Of Addiction
Be it substance abuse, or a specific behavioral issue, addiction is a chronic disease that can potentially affect anyone but most typically affects a subset of people whose circumstances correlate to a basic list of risk factors. This is because addiction is a disease born most often from stress and trauma.
These risk factors, which make a child more likely to fall victim to drug use in later years as per the National Institute on Drug Abuse (NIDA), include (but are not limited to):
- Early aggressive behavior.
- Lack of parental supervision.
- Addicted friends.
- Drug availability.
- Socio-economic circumstances.
These are all risk factors that occur in different domains, ranging from an individual domain to the domain of a household, community, or group of friends. According to the Mayo Clinic, other factors include anxiety and depression, a family history of addiction, and an existing mental health disorder.
Note that correlation and causation are not the same thing. You can have one or all of the above accurately describe your mental state and still be a sober individual without an addiction problem. Likewise, you could have had a perfectly happy childhood in a healthy environment with a family with no known chronic conditions or mental issues and still become physically dependent on alcohol or another drug out of other circumstances.
But while each unique case requires a unique individual approach, understanding prevention and the best way to apply preventative measures requires understanding what sort of a mental and emotional state is most likely to lead to addiction in a person.
In this case, the prevailing denominator across all levels is excessive stress. As per a study on chronic stress and vulnerability, stress can lead to substance abuse and is a well-known risk factor, with more concrete evidence appearing annually.
This is because, to put it simply, the antidote to stress is pleasure, and addictive substances or behaviors worm their way into our lives because they offer instant pleasure. However, that is also what makes them dangerous.
Stopping Addiction In Its Tracks
When you take a drug, gamble, or watch porn as an addict, the response in your brain is immediate release – and subsequent withdrawal, craving for another “hit.” Addiction is a behavioral disease that manifests when your natural reward system – what keeps you alive and allows you to learn through rewarding choices – is exploited by an unnaturally effective release of happiness neurotransmitters like dopamine.
This is why co-opting that reward system with exercise, a healthy support system – and medication in severe substance abuse cases – is critical to slowly bring the mind back to the point where it stops craving constant release.
Reducing stress, in this case, speeds up the process because it partially eliminates the point of release, to begin with. This is why many treatment options for severe cases of addiction recommend an inpatient program to remove the temptation and possible stressors. But what works as part of the basic tenets of treatment also works in prevention.
To stop addiction from developing, it’s important to knock the legs out from under it. This requires a multi-pronged approach, which may include (but is not limited to):
- Effective communication in the household: A poor relationship between a parent and a child can foster many problems, including addiction. Furthermore, parents who reject who their children are can foster and create stress and depression.
- Quality drug education in the community: The effects of drugs – both on relationships and individuals – need to be stressed.
- Addiction role models: Stay clean for your kids if you’re a recovering addict. Other recovering addicts can help curb addiction and promote recovery through success stories. As per HealthyPlace.com, strong support groups help keep recovering addicts sober.
Preventing An Addiction Relapse
Effective measures of prevention are needed to reduce the rate of addiction in society and hopefully improve an individual’s mental and emotional state to the point where drug addiction is, at the very least, unlikely to develop – but even after someone begins to become addicted, there’s another form of prevention that needs to be practiced: The prevention of a relapse. Drug relapses are more common than some might think – in fact, most people relapse, even after successful treatment, as per the NIDA. That isn’t because the treatment didn’t work or because of a lack of willpower on the part of most addicts – it’s because addiction is a chronic disease, and undergoing detox and surviving rehab doesn’t cure a person of its effects.
As such, some tips for preventing relapse include (but are not limited to):
- Finding a treatment plan to stick with.
- Staying away from old stimuli.
- Building and maintaining a strong support system.
- Finding healthy alternative methods of stress release.
Even with these preventative measures, relapse is always a possibility. It’s important for addicts and their loved ones to know that relapses are never grounds for disappointment – sadly, they are all too often par for the course. The only solution is to get back onto the horse and move on.
Prevention, Intervention, Treatment
With addiction, looking at things comprehensively helps a lot. Addiction is rarely alone – it’s often paired with mental conditions like severe depression or bipolar disease, as per DrugAbuse.gov, and may help mask the symptoms of another, deeper issue.
Likewise, prevention shouldn’t be seen as separate from intervention or treatment. All three are part of a larger, comprehensive approach to tackling addiction – both from the side of the addict and their loved ones. Always remember that recovery is never definitive or mirrored from one individual to the next – everyone travels their unique path to self-improvement, and cookie-cutter solutions only present incomplete treatments.
When Prevention Fails
Prevention can fail. When it does, it’s important to know why. The first possible reason is that outliers exist even with positive, inclusive prevention methods. In some cases, addiction may have already progressed to a point where simply taking preventative measures is no longer effective.
And finally, there’s always the possibility that prevention is not an option. There are countless people out there at risk of developing an addiction without the means to change their lives on their own. And ever after addiction is addressed, peer support becomes integral to keeping the recovery going.
Communities need to step in and provide relief to their inhabitants, curbing addiction with an understanding of the disease, a proper diagnosis of its symptoms, and resources to help recovering addicts support each other locally and stay away from each other’s vices.
Sources:
- Drug Policy Alliance. Mass Incarceration and Criminalization. Drug Policy Alliance. Accessed October 15, 2022. https://drugpolicy.org/issues/mass-criminalization
- National Institute on Drug Abuse. What are risk factors and protective factors? National Institute on Drug Abuse. Published October 2011. Accessed October 15, 2022. https://nida.nih.gov/publications/preventing-drug-use-among-children-adolescents/chapter-1-risk-factors-protective-factors/what-are-risk-factors
- Mayo Clinic. Drug addiction (substance use disorder) – Symptoms and causes. Mayo Clinic. Published October 4, 2022. Accessed October 15, 2022. https://www.mayoclinic.org/diseases-conditions/drug-addiction/symptoms-causes/syc-20365112
- Sinha R. Chronic Stress, Drug Use, and Vulnerability to Addiction. Annals of the New York Academy of Sciences. 2008;1141:105. doi:10.1196/annals.1441.030
- Tracy N. Importance of Drug Addiction Support | HealthyPlace. Published December 29, 2021. Accessed October 15, 2022. https://www.healthyplace.com/addictions/drug-addiction/importance-of-drug-addiction-support
- National Institute on Drug Abuse. Treatment and Recovery. National Institute on Drug Abuse. Published July 2020. Accessed October 15, 2022. https://nida.nih.gov/publications/drugs-brains-behavior-science-addiction/treatment-recovery
- National Institute on Drug Abuse. Introduction. National Institute on Drug Abuse. Published April 2020. Accessed October 15, 2022. https://nida.nih.gov/publications/research-reports/common-comorbidities-substance-use-disorders/introduction
The Heights Treatment Editorial Guidelines
There is a vast amount of misinformation online especially as it relates to health & wellness. We have made it our mission at The Heights Treatment to provide accurate, medically sound content that has been medically reviewed by a doctorate level clinician so that you can trust the information contained within our website.